Background:The standard treatment for Hodgkin lymphoma (HL) patients presenting a relapsed/refractory (R/R) disease is salvage chemotherapy followed by autologous stem cell transplantation (ASCT). However, with commonly used chemotherapy combinations (such as DHAP, ICE, BEGEV), 25-30% of these patients fail to achieve a complete metabolic response (CMR) and to proceed to ASCT, with subsequently poor outcomes. Single agents brentuximab vedotin (BV) and pembrolizumab have shown efficacy in heavily pretreated HL patients, as reported in previous studies. The combination of BV with nivolumab has been explored in a phase 1/2 study as first salvage treatment for HL patients, showing a CR rate of 61% (Herrera et al 2018). We explored the outcome of BV and pembrolizumab combination as salvage treatment in a series of R/R HL patients.
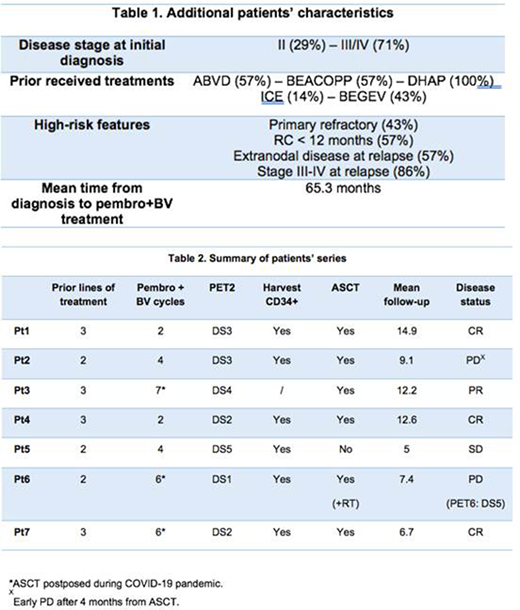
Methods:We retrospectively collected data of seven HL patients presenting with a high-risk multi-refractory disease (two or more prior treatments) followed at Jules Bordet Institute between May 2019 and July 2020 and treated with a combination of BV and pembrolizumab. Patients were covered by special insurance conditions allowing treatment reimbursement. Treatment proposal was approved by a local multidisciplinary committee. Treatment consisted of 3-week cycles with a combination of BV (1.8 mg/kg IV) and pembrolizumab (200 mg IV fixed dose), an early PET-CT evaluation followed by high-dose chemotherapy and ASCT consolidation for those achieving a Deauville score ≤4. After ASCT, patients received BV as maintenance for a total of 16 administration (including pre-ASCT cycles).
Results:We included 7 patients, 6 male and 1 female, with a mean age of 27.4 (20.6-36.3) years. All patients presented with an advanced-stage disease, with a mean number of 2.56 (2-3) prior treatments. The median follow-up time was 9.7 months, while the average number of received cycles of treatment was 4.2 (range 2-7). Table 1 shows additional patients' characteristics. The overall response rate (ORR) was 87% and particularly a CR was achieved in five patients (72%), with a median time to response of two cycles. One partial response and one disease progression were also observed. Six patients proceeded to ASCT (86%) and subsequent BV maintenance, with one early disease progression. One patient, in complete molecular remission after 2 cycles, locally progressed after 6 cycles and received radiotherapy before ASCT.
Table 2 summarizes the outcome for each patient included in the series.
Conclusions:The BV and pembrolizumab combination is a very effective bridge treatment to ASCT for high-risk R/R HL patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal